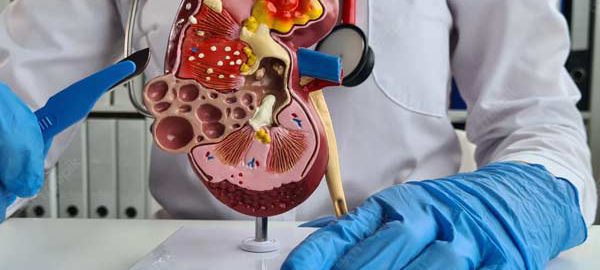
What is bile duct surgery?
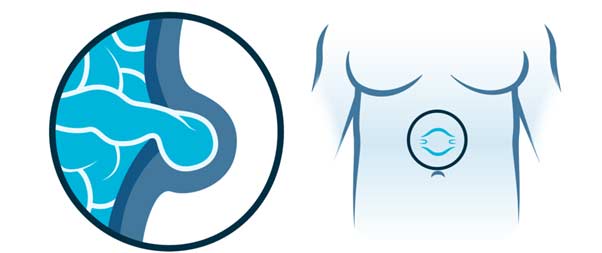
The bile ducts connect the liver with the gallbladder and the small intestine. Surgery is carried out to remove the part of the bile duct that contains the tumor, both malignant and benign. Surgery may also be recommended to prevent complications or because of the possibility of malignancy.
Sometimes, in addition to the resection of the bile duct, it must be associated with the removal of a part of the liver.
Redrainage of bile from the liver is done using a loop of intestine sewn into the bile duct that remains in the liver.
Previous considerations.
Before any surgery, an assessment should be carried out by the anesthetist where they will advise you which medication you should stop taking and which you should continue taking. Sometimes you must be evaluated by another specialist if you have underlying diseases.
In the case of anticoagulant treatment or treatment that facilitates bleeding, the anesthesiologist, haematologist, cardiologist or family doctor will inform about the attitude to follow.
Normally you should be evaluated by Hematology before the intervention since they must draw blood to study your blood group and make a reserve of blood bags for the day of the intervention. In this surgery, bleeding is an important complication, so we must offer you maximum safety. For your peace of mind, most of our patients do not require a blood transfusion.
In the case of smoking, the habit should be stopped because it facilitates anesthetic management, smoker patients have more complications than smokers in anesthetic procedures.
It is recommended to perform moderate-intensity exercise before any intervention, unless there is a specific contraindication, such as walking at least 60 minutes a day.
How is the preparation prior to the intervention?
FOOD AND MEDICINE
In preparation for a hepatectomy, your surgeon may ask you to:
- Do not eat anything before surgery. You may have a sip of water with your medications, but avoid eating and drinking for at least six hours before surgery.
- Discontinue certain medications and supplements. Talk to your doctor about all medications and supplements you take. You continue to take most medications as directed by your doctor. Your doctor may ask you to stop certain medications and supplements because they can increase your risk of bleeding.
How is the surgery performed? (type of incision, resection, type of drainage, anesthesia)
BEFORE THE INTERVENTION
Bile duct surgery is performed under general anesthesia, so you won’t be conscious during the procedure. Numbing medications are given intravenously into the arm. Once the medications take effect, your health care team will insert a tube down your throat to help you breathe, place a catheter to monitor your urine, and place lines in your neck and wrist to administer drugs and learn about your heart function.
You may have an epidural catheter or injection into your spine, as well as local nerve blocks in your abdominal wall. These procedures allow you to recover with minimal pain and discomfort after surgery and help reduce the amount of opioid pain medication you’ll need.
Your surgeon will perform bile duct surgery using a laparoscopic or open procedure.
DURING THE PROCEDURE
Depending on your situation, your surgeon will recommend one of two surgical approaches:
Bile duct surgery with a minimally invasive approach (laparoscopic)
This approach route is used in very selected cases since the technical difficulty is very high. The surgeon makes four to six small incisions in the abdomen. A tube with a tiny video camera is inserted into your abdomen through one of the incisions. The surgeon watches a video monitor in the operating room while using surgical tools inserted through the other incisions in the abdomen to remove the diseased part of the bile duct.
One of the incisions will be enlarged to extract the excised piece. The incisions are then sutured and you are moved to a recovery area. A laparoscopic biliary surgery takes between three and six hours. Very specialized instruments are used to prevent bleeding during the intervention.
In some cases, the surgeon may start with a laparoscopic approach and determine that a larger incision is necessary due to scar tissue from operations, previous complications, or an inability to safely continue with the procedure.
Bile duct surgery with traditional (open) approach.
The surgeon makes an incision about 20 centimeters in the abdomen below the ribs on the right side. Muscle and tissue are retracted to reveal the liver and bile duct. Sometimes, in addition to the resection of the bile duct, it must be associated with the removal of a part of the liver. Redrainage of bile from the liver is done using a loop of intestine sewn into the bile duct that remains in the liver.
The incision is sutured and you are transferred to a post-anesthetic recovery area. An open cholecystectomy takes between three and six hours. Very specialized instruments are used to prevent bleeding during the intervention. It is usually performed when the procedure cannot be carried out with maximum safety through the laparoscopic approach due to the complexity of the case.
Sometimes it is necessary to place a tube or drain inside the abdomen with an outlet through the skin to allow the discharge of fluid from the area where the diseased part of the liver was. This tube will be removed before discharge home, with exceptions.
What happens after the surgery?
After surgery, the patient is transferred to the Intensive Care Unit (ICU) where he will remain for 24 hours if there are no incidents. It is possible that the anesthesiologist will remove the connection to a breathing machine in the operating room or the doctor in charge of your surveillance in the ICU will do it. You will slowly wake up from the effects of the anesthetic drugs so you may have a feeling of not remembering the process. After your stay in this unit you will then be transferred to your room.
HOW IS THE RECOVERY IN THE HOSPITAL?
It is possible to feel nausea or abdominal pain after the intervention but they will be controlled with the prescribed medication. After about 24 hours, he will begin with the intake of liquids and the next day solid foods. We recommend sitting down and starting to walk about 24 hours after the intervention. The catheter that is inserted into your bladder will be removed in 1 or 2 days. At all times you will be supervised and helped by nursing staff.
If your surgery progresses on the floor without any incident, you will remain hospitalized for between 5 and 10 days.
HOW IS THE RECOVERY AT HOME?
Our premise is to be active in recovery. For this reason, we encourage the patient to walk daily, we recommend walking at least 60 minutes each day both inside and outside the house. Important physical efforts that may affect wound healing should always be avoided.
When you are discharged home, you will be prescribed medication to make you feel as comfortable as possible. You will resume your previous medication following the surgeon’s recommendations, since some drug may not be recommended in the first days after surgery. Normally the taking of painkillers is indicated to control the pain and the injection of heparin to avoid the appearance of thrombi in your legs.
In relation to food, we recommend the first week to avoid copious and fat-rich meals. Subsequently, all types of food will be progressively reintroduced, with possible intolerance of some of them, so their intake will be suspended and they will be tried again in the following weeks. Occasionally diarrhea may appear that usually lasts a few days or a week in relation to the new situation of the digestive system.
You can wet your wounds when you wash yourself and then gently dry them with the application of any antiseptic (chlorhexidine, povidone-iodine, crystalmine…). These wounds should be evaluated by nursing around 7 and 10 days after surgery.
Virtually full recovery can take approximately three to four weeks in laparoscopic surgery. However, in open surgery, once at home, full recovery can take four to six weeks. It will depend on your physical condition before surgery and the complexity of the operation.
What are the risks of bile duct surgery?
Bile duct surgery is a technically difficult surgery, even more so if it is associated with the removal of part of the liver, and requires significant experience on the part of the surgeon. Extensive research shows that surgeries result in fewer complications when performed by highly experienced surgeons at centers that perform many of these operations.
Infrequent and frequent risks : Infection or bleeding of the surgical wound, acute urinary retention, phlebitis, intestinal rhythm disorders. Prolonged pain in the area of the operation.
Infrequent and serious risks: Dehiscence of the laparotomy (opening of the wound). Biliary fistula that in most cases resolves with medical treatment (medicines, serums, etc.), but sometimes requires other tests (ERCP and/or bile drainage). Intra-abdominal bleeding or infection. Intestinal obstruction. Narrowing of the bile duct. Cholangitis (infection of the bile ducts). Reproduction of the disease.
These complications are usually resolved with medical treatment (medicines, serums, etc.), but they may require a reoperation, usually an emergency, and in exceptional cases death may occur.