What is colectomy?
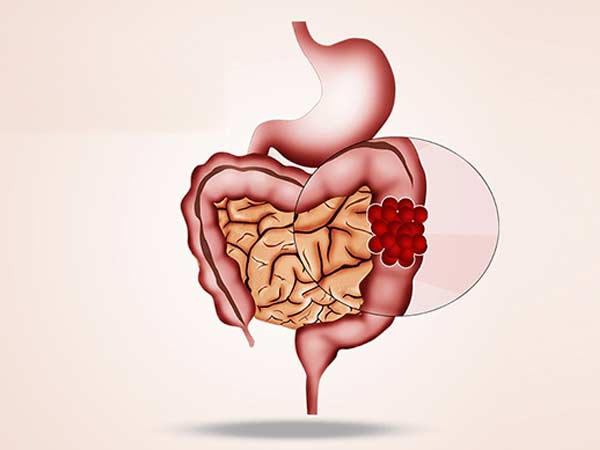
Colectomy is a surgical procedure in which all or part of the colon is removed. The colon, also known as the large intestine, is a long, tube-shaped organ at the end of the digestive tract.
There are several types of colectomy operations:
- Total colectomy involves removal of the entire colon.
- Partial colectomy involves the removal of part of the colon.
- Hemicolectomy involves removal of the right or left part of the colon.
- Proctocolectomy involves removal of both the colon and the rectum.
Colectomy surgery often requires other procedures to reconnect the remaining parts of the digestive system and allow waste to pass out of the body.
Colectomy is used to treat and prevent diseases and disorders that affect the colon, such as:
- Uncontrollable bleeding. Heavy bleeding from the colon may require surgery to remove the affected part of the colon.
- Intestinal obstruction. A blocked colon is an emergency that may require a full or partial colectomy, depending on the situation.
- Colon cancer. Early-stage colon cancer may require removal of only part of the colon during colectomy. More advanced cancer may require removal of a larger portion of the colon.
- Crohn’s disease. If medications don’t help, removal of the affected part of the colon may offer a resolution of your signs and symptoms. Colectomy may also be an option if precancerous changes are found during a test to examine the colon (colonoscopy).
- Ulcerative colitis. Your doctor may recommend a total colectomy if medications don’t help control your signs and symptoms. Colectomy may also be an option if precancerous changes are found during a colonoscopy.
- Your doctor may recommend surgery to remove the affected part of your colon if your diverticulitis recurs or if you develop complications.
- preventive surgery. If you are at very high risk of colon cancer due to the formation of multiple precancerous colon polyps, you may choose to have a total colectomy to prevent cancer in the future. Colectomy may be an option for people with inherited genetic disorders that increase the risk of colon cancer, such as familial adenomatous polyposis or Lynch syndrome.
Previous considerations
Before any surgery, an assessment should be carried out by the anesthetist where they will advise you which medication you should stop taking and which you should continue taking. Sometimes you must be evaluated by another specialist if you have underlying diseases.
In the case of anticoagulant treatment or treatment that facilitates bleeding, the anesthesiologist, haematologist, cardiologist or family doctor will inform about the attitude to follow.
Normally you should be evaluated by Hematology before the intervention since they must draw blood to study your blood group and make a reserve of blood bags for the day of the intervention. In this surgery, bleeding is an important complication, so we must offer you maximum safety. For your peace of mind, most of our patients do not require a blood transfusion.
In the case of smoking, the habit should be stopped because it facilitates anesthetic management, smoker patients have more complications than smokers in anesthetic procedures.
It is recommended to perform moderate-intensity exercise before any intervention, unless there is a specific contraindication, such as walking at least 60 minutes a day.
How is the preparation prior to the intervention?
FOOD AND MEDICINE
In preparation for a cholecystectomy, your surgeon may ask you to:
- Do not eat anything before surgery. You may have a sip of water with your medications, but avoid eating and drinking for at least six hours before surgery.
- Discontinue certain medications and supplements. Talk to your doctor about all medications and supplements you take. You continue to take most medications as directed by your doctor. Your doctor may ask you to stop certain medications and supplements because they can increase your risk of bleeding.
- Drink a solution to cleanse the intestine. Your doctor may prescribe a laxative solution to mix with water at home. Drink the solution over a period of several hours, as directed. The solution causes diarrhea to help you empty your colon. Your doctor may also recommend that you take enemas.
It is not always possible to prepare for a colectomy. For example, if you need an emergency colectomy for a blockage or perforation in your intestine, you may not have time to prepare.
How is the surgery performed? (type of incision, resection, type of drainage, anesthesia)
BEFORE THE INTERVENTION
A colectomy is performed under general anesthesia, so you will not be conscious during the procedure. Numbing medications are given intravenously into the arm. Once the medications take effect, your health care team will insert a tube down your throat to help you breathe and place a catheter to monitor your urine.
DURING THE PROCEDURE
Depending on your situation, your surgeon will recommend one of two surgical approaches:
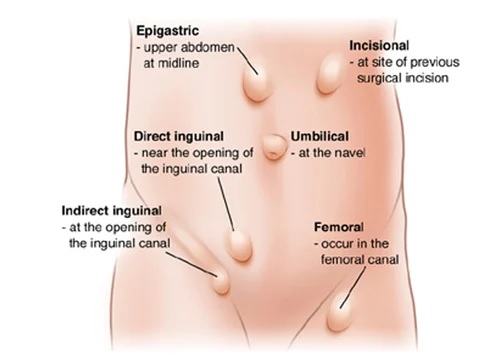
- open colectomy. In open surgery, a longer incision is made in the abdomen to access the colon. The surgeon uses surgical tools to free the colon from the surrounding tissue and cuts out a part of the colon or the entire colon.
- laparoscopic colectomy. In a laparoscopic colectomy, also called a “minimally invasive colectomy,” several small incisions are made in the abdomen. The surgeon inserts a tiny video camera through one incision and certain special surgical tools through the other incisions.
The surgeon watches a video screen in the operating room as tools are used to free the colon from surrounding tissue. The colon is then removed through a small incision in the abdomen.
Laparoscopic colectomy relieves pain and reduces recovery time after surgery. But not everyone is a candidate for this procedure. Also, in some situations, the operation may begin as a laparoscopic colectomy, but circumstances may require the surgical team to convert it to an open colectomy.
Once the colon has been repaired or removed, the surgeon will reconnect the digestive system so that the body can expel waste. Options include the following:
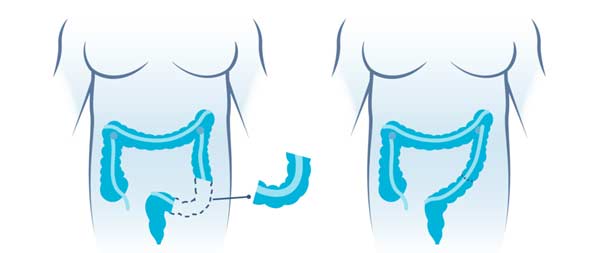
- Union of the remaining parts of the colon. Typically, the surgeon joins the remaining parts of the colon together to create what is called an “anastomosis.” In this way, the stool will leave the body just as it did before.
- Connection of the intestine with an opening created in the abdomen. The surgeon may connect the colon (colostomy) or small intestine (ileostomy) to an opening created in the abdomen. This allows waste to pass out of the body through the opening (stoma). You must use a bag outside the stoma to collect stool. This can be permanent or temporary.
- Connection of the small intestine with the anus. After removing the colon and rectum (proctocolectomy), the surgeon may use a part of the small intestine to create a sac that connects to the anus (ileoanal anastomosis). This allows you to pass waste normally, although you may have several liquid bowel movements every day.
As part of this procedure, you may need to have a temporary ileostomy.
The surgeon will discuss the options with you before the operation.
Sometimes it is necessary to place a tube or drain inside the abdomen with an outlet through the skin to allow the discharge of fluid from the area where the node was. This tube will be removed prior to discharge home.
What happens after the surgery?
After surgery, the patient slowly awakens from the effects of the anesthetic drugs, so they may have a feeling of not remembering the process. You will be for a short period of time in an area called post-anesthetic recovery or Intensive Care Unit for greater surveillance if your situation requires it. You will then be transferred to your room.
HOW IS THE RECOVERY IN THE HOSPITAL?
It is possible to feel nausea or abdominal pain after the intervention but they will be controlled with the prescribed medication. After about 24 hours, you will begin with the intake of liquids and then solid foods in the following days. We recommend sitting down and starting to walk about 24 hours after the intervention. The catheter that is inserted into your bladder will be removed in 1 or 2 days. At all times you will be supervised and helped by nursing staff.
If the surgeon has finally performed a stoma, you and your companion will receive the necessary information and training for its management.
If your surgery progresses on the floor without any incident, you will remain hospitalized for between 5 and 7 days.
HOW IS THE RECOVERY AT HOME?
Our premise is to be active in recovery. For this reason, we encourage the patient to walk daily, we recommend walking at least 60 minutes each day both inside and outside the house. Important physical efforts that may affect wound healing should always be avoided.
When you are discharged home, you will be prescribed medication to make you feel as comfortable as possible. You will resume your previous medication following the surgeon’s recommendations, since some drug may not be recommended in the first days after surgery. Normally the taking of painkillers is indicated to control the pain and the injection of heparin to avoid the appearance of thrombi in your legs.
In relation to food, we recommend a soft diet for the first week and avoid copious meals. Subsequently, all types of food will be progressively reintroduced, being fundamental those rich in fiber such as vegetables and fruit. You must be well hydrated so we recommend that you drink at least 1.5 liters of non-carbonated liquids. Occasionally diarrhea may appear that usually lasts a few days or a week in relation to the new situation of the digestive system.
You can wet your wounds when you wash yourself and then gently dry them with the application of any antiseptic (chlorhexidine, povidone-iodine, crystalmine…). These wounds should be evaluated by nursing around 7 and 10 days after surgery.
If you have had an opening from the intestine to your abdominal wall, we will facilitate contact with a specialized nurse (stomatherapist) in the management of the stoma who will help you and resolve all kinds of doubts.
Virtually full recovery can take approximately three to four weeks for laparoscopic colectomy. However, with open colectomy, once at home, full recovery may take four to six weeks. It will depend on your physical condition before surgery and the complexity of the operation.
What are the risks of colectomy?
The normal thing is that your intervention proceeds without incidents but you must know the potential complications.
Less serious and frequent risks: Infection or bleeding of the wound, acute retention of urine, phlebitis. Increased number of stools. Prolonged pain in the area of the operation. Laparoscopic surgery may cause gas extension to the subcutaneous tissue or other areas and referred pain, usually to the shoulder.
Infrequent and serious risks: Fistula of the anastomosis due to impaired healing that in most cases is resolved with medical treatment (medications, serums, etc.), but that sometimes requires a reoperation with the creation of an artificial anus. Intra-abdominal bleeding or infection. Intestinal obstruction. Reproduction of the disease. Due to laparoscopic surgery, there may be vascular injuries, injuries to neighboring organs, gas embolism and pneumothorax.
These complications are usually resolved with medical treatment (medicines, serums, etc.), but they may require a reoperation, usually an emergency, and in exceptional cases death may occur.
Your risk of complications depends on your overall health and the reason you’re having a colectomy.